In September 2024, the U.S. Food and Drug Administration (FDA) issued an urgent alert following Pfizer’s decision to voluntarily withdraw Oxbryta (voxelotor) from the market. This recall came after alarming findings from postmarketing studies linking sickle cell disease treatment to severe side effects, including increased rates of vaso-occlusive crises (VOCs), hospitalization, and even death.
These safety concerns outweighed the medication's benefits, prompting Pfizer to halt distribution and discontinue all ongoing clinical trials.
Multidistrict Litigation (MDL) Details
- A federal mass tort is forming following Pfizer’s voluntary global recall of Oxbryta (voxelotor) in September 2024
- The recall followed safety data linking Oxbryta to increased vaso-occlusive crises (VOCs), hospitalizations, strokes, and fatalities in sickle cell patients
- Multiple product liability and wrongful-death suits have been filed against Pfizer and Global Blood Therapeutics
Cases We’re Currently Accepting
- Individuals who were prescribed or participated in clinical trials for Oxbryta
- Claimants with adverse events including:
- Increased VOCs or pain crises
- Stroke or neurological injury
- Hospitalization from treatment complications
- Death potentially linked to Oxbryta use
Recent Key Litigation Developments
- January–March 2025: Surge in filings, including wrongful-death suits and claims of malfunctioning design/marketing
- June 2025: Bellwether trials scheduled—first set for June 7, 2027, another in August 2027
- Ongoing litigation includes claims of fraudulent concealment, tolling of limitations, and combined product-plus-medical negligence suits
The Parties’ Litigation Positions
- Plaintiffs: Allege that manufacturers aggressively promoted Oxbryta as safe and effective while failing to disclose real-world evidence of serious risks (VOCs, stroke, death)
- Defendants: Likely to defend on the basis of FDA-approved labeling, contend causation is unproven, and may argue risks were outweighed by benefits
Settlement Potentials
- No settlements reported as of mid‑2025
- Potential mid‑ to high-six-figure payouts per individual, possibly scaling higher in wrongful-death cases
- Expect settlement activity to ramp up in the year before the 2027 bellwether trials, as internal documents become discoverable
Major Concerns / Expectations
- Limited timeframe: Statutes of limitation began with the September 2024 recall; timely filing is crucial
- Evidence emerging: Postmarketing and trial-phase data raise serious causation concerns
- Trial schedules set: Bellwethers in mid‑2027 will significantly affect pending claim values and patterns
- Multi-pronged claims: Plaintiffs may assert both product defect/failure-to-warn and medical malpractice, particularly in hospital-prescribed contexts

This sudden development has raised questions about what to do next for patients and families who rely on Oxbryta to manage the debilitating effects of sickle cell disease. The FDA advises patients to stop using Oxbryta and consult their healthcare providers for alternative treatments. For those who suffered harm due to the drug, there may also be legal options available. Oxbryta’s side effects victims could be entitled to compensation for medical expenses, pain and suffering, and other losses.
Updates on the Oxbryta Lawsuit (November 2025)

November 1, 2025 - First Settlement Reached as More Families Come Forward
The Oxbryta litigation has reached an important milestone. This month, at least one lawsuit against Pfizer Inc. and Global Blood Therapeutics has reportedly settled in federal court. A Notice of Settlement was filed in the Northern District of California, though the details remain confidential, as is typical in pharmaceutical product liability cases.
While this doesn’t signal a global resolution, it does suggest that settlement discussions are active and that Pfizer may be willing to resolve individual claims under the right circumstances.
New Cases Filed as Settlement Talks Continue
Oxbryta was marketed as a breakthrough treatment for sickle cell disease (SCD), but families continue to come forward alleging that the drug caused serious side effects, including life-threatening vaso-occlusive crises (VOCs). In one recent case, the parents of a young child claim their son nearly died multiple times while on Oxbryta and required critical care treatment. Their lawsuit seeks compensation for medical costs, pain and suffering, and long-term impacts on the child’s health.
Pfizer’s Own Statement Raises Questions
While Pfizer continues to deny liability in these cases, one of the most notable developments is the company’s public acknowledgment that “the overall benefit of Oxbryta no longer outweighs the risk.” That admission came around the time Oxbryta was voluntarily withdrawn from the global market in 2024 following troubling post-marketing data.
For plaintiffs and their lawyers, this statement may carry weight in ongoing settlement discussions, especially as more cases highlight the disconnect between Oxbryta’s early marketing promises and the real-world complications patients have suffered.
As more families continue to evaluate their legal options, all eyes will be on whether Pfizer chooses to quietly settle these claims—or fight them one by one in court.
October 1, 2025 - Mediation Begins as Pfizer Faces Broader Sickle Cell Setbacks
The Oxbryta lawsuits are moving into a critical new phase. Mediation was scheduled to begin on September 9, 2025, with retired Judge Philip S. Gutierrez overseeing settlement talks between plaintiffs and defendants. While there’s no guarantee of a resolution, and the initial mediation did not result in a global settlement, the start of formal negotiations signals real progress in this relatively small but focused litigation.
Why the Size of the Litigation Matters
Unlike large mass torts involving thousands of claims, the Oxbryta docket remains manageable. For plaintiffs, this is often a strategic advantage. With fewer cases in the system:
- Judges can resolve key issues more quickly
- Discovery is less chaotic
- Settlement discussions are more focused
- Individual patient’s stories are less likely to be overlooked
Smaller dockets also reduce the overall financial burden on defendants, making it more likely that fair settlement offers can be made without years of delays.
Pfizer’s Broader Sickle Cell Drug Portfolio Under Pressure
Meanwhile, Pfizer continues to face challenges related to its $5.4 billion acquisition of Global Blood Therapeutics, the company that created Oxbryta:
- Inclacumab failed its Phase III trial, showing no significant benefit in reducing vaso-occlusive crises.
- Osivelotor, another drug acquired in the deal, is now on FDA clinical hold, though the agency has not disclosed specific reasons.
These setbacks raise additional questions about the due diligence and long-term strategy behind Pfizer’s sickle cell investments and may support the plaintiffs’ arguments in the Oxbryta litigation.
September 1, 2025 - Settlement Talks Ordered as Pfizer Faces Another Sickle Cell Setback
The legal fallout from Pfizer’s troubled sickle cell portfolio is gaining momentum. A federal judge has now ordered formal settlement negotiations in the growing wave of lawsuits over Oxbryta, the sickle cell disease drug pulled from the market in 2024 amid safety concerns.
Settlement Negotiations Begin September 2025
On August 18, 2025, Judge Trina L. Thompson appointed retired Judge Philip S. Gutierrez to mediate the Oxbryta litigation. Both sides have been ordered to begin settlement talks on September 9, signaling that the court is moving the proceedings beyond procedural motions and toward potential resolution.
This development marks a major turning point in the litigation. Until now, the lawsuits filed by patients and families who allege serious complications or wrongful deaths linked to Oxbryta have been in early stages. The court’s move suggests growing pressure on both sides to negotiate seriously.
Pfizer’s New Drug Trial Fails, Fueling Scrutiny
Just days earlier, Pfizer announced that inclacumab, a sickle cell drug it had been testing in late-stage trials, failed to meet key benchmarks. The drug showed no meaningful reduction in vaso-occlusive crises (VOCs) compared to placebo, effectively ending its path to approval.
The timing is significant. Inclacumab was one of the key assets Pfizer acquired in its $5.4 billion purchase of Global Blood Therapeutics, the same company that developed Oxbryta. That deal has come under increasing scrutiny since Oxbryta was withdrawn from the global market in 2024 after post-marketing data revealed a higher rate of VOCs and deaths among users.
Implications for the Litigation
While inclacumab never made it to market, its failure supports a broader narrative emerging in the lawsuits: that Pfizer's acquisition strategy may have prioritized market potential over patient safety. For attorneys representing plaintiffs, the recent drug trial failure could help paint a picture of a company that overlooked red flags, not only with Oxbryta but with its entire sickle cell pipeline.
Plaintiffs in these cases allege that Pfizer and Global Blood Therapeutics misrepresented Oxbryta’s safety and efficacy, and continued to promote the drug despite evidence of serious risks. With the court-ordered mediation now underway, attention will shift toward whether Pfizer is prepared to offer meaningful settlements or if this litigation is headed for trial.If you or a loved one was harmed by taking Oxbryta according to a doctor’s prescription, you may be eligible to take legal action and recover compensation to help cover your losses. The Lawsuit Legal News team can answer your questions during a free consultation.
August 1, 2025 - Oxbryta Lawsuits Gaining Momentum as Pfizer Faces Mounting Legal Pressure
Pfizer and its subsidiary Global Blood Therapeutics face increased legal scrutiny over Oxbryta, the now-recalled drug for sickle cell disease. A recent lawsuit filed by a North Carolina family in New York County Supreme Court adds to the growing number of product liability claims alleging that Oxbryta caused serious medical complications, including vaso-occlusive crises (VOCs).
New Injury Claims Filed in New York State Court
- The North Carolina plaintiff alleges that Oxbryta directly caused them to suffer VOCs in July 2024, despite the drug being marketed as a treatment to reduce these exact episodes.
- The lawsuit is one of the first filed in state court rather than in federal court, complicating Pfizer’s efforts to consolidate these cases.
- Pfizer is seeking to move this and other cases into a potential multidistrict litigation (MDL), but because its principal place of business is in New York, removing this case may be more difficult.
MDL Consolidation May Be on the Horizon
There is growing discussion around forming an Oxbryta MDL, which would group individual injury lawsuits before a single federal judge to coordinate pretrial proceedings. A judge already handling one of the pending Oxbryta cases has acknowledged that consolidation may now be appropriate.
Why this matters:
- An MDL could streamline the litigation process for patients harmed by Oxbryta.
- It could also increase pressure on Pfizer to settle claims or respond to common allegations more efficiently.
Legal experts caution that MDL consolidation doesn't guarantee higher compensation. For some plaintiffs, individual state court claims might result in more favorable outcomes, depending on the circumstances.
Oxbryta Recall Class Action Update: Trial Scheduled for 2027
Separate from the personal injury cases, Pfizer is also defending a class action lawsuit tied to its September 2024 recall of Oxbryta. A judge has appointed a mediator to oversee ongoing settlement negotiations, with a trial currently scheduled for August 2027.
While class action outcomes typically don’t directly impact personal injury claims, any settlement or verdict could significantly shape how Pfizer responds to individual lawsuits going forward.
Why Oxbryta’s Market Withdrawal Matters
Unlike many drugs at the center of mass tort litigation, Oxbryta was voluntarily withdrawn from global markets in 2024 after real-world data revealed a higher rate of VOCs and fatalities in users compared to those taking placebo drugs.
This doesn’t mean Pfizer has admitted liability—but the recall is rare and may influence how courts and juries view the company’s handling of the drug’s risks.
July 1, 2025 - New Oxbryta Wrongful Death Lawsuit Filed in California
A new product liability lawsuit has been filed against the makers of Oxbryta, a prescription medication for sickle cell disease (SCD), following the drug’s voluntary market withdrawal in 2024. The plaintiff is a Tennessee widow who alleges the drug caused her husband’s death and that the related pharmaceutical companies failed to warn about life-threatening risks.
Key Allegations in the Oxbryta Lawsuit
- Filed in: U.S. District Court for the Northern District of California
- Defendants: Global Blood Therapeutics and Pfizer
- Plaintiff: The widow and personal representative of a 62-year-old Tennessee man
- Injury Claims on behalf of her husband:
- Worsening of vaso-occlusive crises (VOCs)
- Stroke in April 2024
- Death in May 2024
The complaint claims the drugmakers misrepresented the safety profile of Oxbryta and failed to disclose post-marketing data indicating serious risks, including decreased oxygen delivery, increased VOCs, and fatal complications.
Although Oxbryta received FDA accelerated approval in 2019 and pediatric approval in 2021, it was finally pulled from the global market in September 2024 after Pfizer reviewed real-world registry data showing:
- Higher rates of VOCs among Oxbryta users compared to the placebo group
- A concerning number of patient deaths, potentially linked to the drug
June 1, 2025 - First Trial Now Set for August 2027
The Oxbryta (voxelotor) mass tort litigation is moving forward, with the first bellwether trial now scheduled for August 16, 2027. While the trial date is more than two years away, this milestone signals meaningful progress in a case that has drawn national attention due to serious safety concerns surrounding a drug marketed for sickle cell disease.
What’s at Stake in the Litigation
Plaintiffs allege that Pfizer knowingly promoted Oxbryta as a safe and effective treatment while failing to disclose significant risks, including stroke, vaso-occlusive crises (VOCs), hospitalization, and even death. If the case goes to trial, it will be the first opportunity for a jury to evaluate this evidence and determine whether Pfizer misled the public. The outcome will likely set the tone for future cases and influence broader litigation strategy.
Will the Case Settle Before Trial?
Mass tort cases frequently settle before reaching trial, particularly when discovery reveals damaging internal information. The LLN team believes that Pfizer may seek to avoid public exposure of sensitive documents, increasing the likelihood of a settlement in the months leading up to the trial.
Background and Drug Withdrawal
Oxbryta was voluntarily withdrawn from the market by Pfizer in 2024. In a recent advisory, the National Institutes of Health (NIH) urged patients who had taken the drug to consult with their healthcare providers about discontinuing its use and exploring alternative treatments. This move has added weight to plaintiffs’ claims and continues to raise public and legal scrutiny.
Key Takeaways
Current Status: The litigation is progressing as expected; plaintiffs with complications from Oxbryta may still be eligible to file claims.
Trial Date: August 16, 2027 – the first bellwether case could shape the future of this litigation.
Allegations: Failure to warn, aggressive marketing, and concealment of life-threatening side effects.
Potential Settlement: A pre-trial resolution remains possible as discovery advances.
May 1, 2025 - California Lawsuit Links Oxbryta to Sickle Cell Patient’s Death Amid Allegations of Defective Drug Design and Medical Negligence
A new lawsuit filed in California highlights growing concerns over the safety of Oxbryta, a drug once promoted as a breakthrough treatment for sickle cell disease. The complaint, brought by an Oakland woman on behalf of herself and her late husband’s estate, alleges that a combination of medical malpractice and a defectively designed drug led to her husband's untimely death in March 2024.
The decedent, a 45-year-old man with a long history of sickle cell complications, reportedly experienced a rapid health decline over several days, culminating in multi-organ failure and cerebral edema. The suit names UCSF Benioff Children’s Hospital Oakland and Alta Bates Summit Medical Center among the healthcare providers accused of failing to diagnose and treat a vaso-occlusive crisis and acute chest syndrome in a timely manner. Critical delays in transferring him to appropriate care, as well as lapses in blood exchange procedures and internal communication, are at the center of the malpractice claims.
In parallel, the complaint targets Global Blood Therapeutics, Pfizer, and The Pfizer Incubator LLC, alleging that Oxbryta was defectively designed and improperly marketed, particularly after the plaintiff’s husband received it during a 2021 clinical trial. The lawsuit cites Pfizer’s voluntary withdrawal of Oxbryta in September 2024, following reports of increased vaso-occlusive crises and patient deaths, as evidence that the drug’s risks were not adequately disclosed.
The lawsuit includes twelve causes of action, spanning negligence, product liability, wrongful death, and false advertising, and seeks both compensatory and punitive damages.
April 1, 2025 - First Trial is Scheduled... But Not Until June 2027
A federal judge has officially scheduled the first Oxbryta lawsuit to go to trial, naming Pfizer and Global Blood Therapeutics as defendants. The trial date is set for June 7, 2027, and it's expected to last roughly 12 to 15 days.
The delay may feel excruciating, but in the world of mass torts, this kind of timeline is totally normal. These cases move at a snail’s pace—bogged down by corporate legal tactics, lengthy discovery, and loads of expert testimony. It’s a slow process, but one that's necessary to hold major pharmaceutical companies accountable for the harm caused by their products.
When the trial kicks off, jurors will hear from medical professionals, doctors who prescribed Oxbryta, and key players from the companies themselves to explain the development, testing, marketing, and prescribing processes used for this drug. The spotlight will be on whether the drugmakers minimized or failed to properly warn patients and providers about the risk of vaso-occlusive crises (VOCs)—a severe and painful complication that impacts people with sickle cell disease.
March 1, 2025 - Almost 5 Months After Pfizer's Voluntary Oxbryta Recall, Injured Patients Are Filing Lawsuits to Cover Their Losses
Last September, Pfizer issued a global recall of its drug, Oxbryta, due to evidence that it increased the risk of vaso-occlusive crises (VOCs) in patients taking the medication. The recall will likely trigger the start of the statute of limitations that applies to personal injury and dangerous drug claims against the manufacturer. This means people harmed by the drug must file their lawsuits within a specific amount of time or lose the right to request compensation for their losses.
Pending claims allege the company knew or should have known about the potential risk of VOCs and other serious medical concerns, including organ failure and strokes. Rather than warning medical providers and patients about these risks, plaintiffs allege Pfizer promoted its drug and concealed its dangers. If you were injured after taking Oxbryta, you need to understand how long you have to bring a claim. The team at LLN can answer all your questions for free.
February 1, 2025 - More Claims Allege Oxbryta Makers Failed to Warn About Known Risks
Patients who experienced serious side effects after taking Oxbryta continue to bring lawsuits against the manufacturers, Pfizer and Global Blood Therapeutics. Reported medical concerns related to Oxbryta use include vaso-occlusive crises (VOCs), organ damage and failure, blood vessel blockage, strokes, and even death. The injured plaintiffs allege these companies knew about the potential risks of this drug but failed to warn patients and doctors until the drug was finally pulled from the shelves in September 2024.
Some lawsuits claim Pfizer fraudulently concealed the dangers of taking Oxbryta and argue the statute of limitations should be tolled by this deliberate behavior. If the evidence supports the fraudulent concealment or active misleading theory, punitive damages could play a large role in these cases. If you have questions about this litigation and whether you qualify to bring a claim, reach out to the Lawsuit Legal News team to learn more.
January 1, 2025 - Recent Study Inconclusive Because More Than 50% of Patients Failed to Follow Through
The American Society of Hematology journal Blood released a study intended to provide real-world evidence of Oxbryta's use and effectiveness. Unfortunately, 31 of the 60 participants did not start the drug, didn't return for requested follow-up labs, or simply refused to take it even after it was approved. Nine more participants only returned for the first month's labs. As a result, the study's findings were based on a small percentage of people and cannot be considered reliable data.
After this study's inconclusive findings and the shocking results of the two studies described in our December 11th report below, Pfizer recalled Oxbryta. At this point, it is no longer available in the US and worldwide. If you used Oxbryta and developed serious medical conditions, you may be eligible to bring a dangerous drug product liability lawsuit. Reach out to the Lawsuit Legal News team to learn more.
December 11, 2024 - Two Studies Show a Giant Increase in Deaths in Oxbryta Patients versus Placebo Group; More Studies Needed to Understand How the Number Could Be So High
Two recent clinical trials evaluating the safety and efficacy of voxelotor (Oxbryta) have raised serious safety concerns and led to the suspension of its use in ongoing studies.
Both studies were conducted in 2024: Study GBT440-032 and Study GBT440-042. Both studies revealed extreme increases in fatalities among participants taking the medication when compared to patients taking a placebo (a placebo is a pill made of sugar or some other useless ingredient that makes the participant think they are taking the drug).
Study GBT440-032 focused on children aged 2 to 15 with sickle cell disease who were at a high risk of stroke. The trial involved 236 participants across multiple countries, including Egypt, Ghana, Kenya, and the United States. In this study, 8 deaths were reported in the group receiving voxelotor (Oxbryta), compared to just 2 in the placebo group.
Study GBT440-042 examined the impact of voxelotor (Oxbryta) on patients aged 12 and older with leg ulcers, a common complication of sickle cell disease. This study examined 88 participants in Brazil, Kenya, and Nigeria. Eight deaths were also reported during the open-label phase of this trial (meaning there was no placebo group, and both the patients and doctors were aware that they were taking the actual medicine).
Despite these studies and their alarming results, definitive evidence still doesn’t exist that voxelotor or Oxbryta directly caused these deaths. Some cases may have been caused by outside factors like infections.
Regardless, the findings have halted any further test trials or follow-up studies and, obviously, the sale of the drug. In September, Pfizer removed this medication from pharmacy shelves and it is no longer available for prescription.
The European Medicines Agency (EMA) is conducting a full review of the data to determine whether the drug can be made available for sale again or permanently revoked. Currently, it is not for sale anywhere in the world, including the United States.
These findings have raised serious doubts about the continuation of the sickle cell treatment drug. Unfortunately, many people took the drug before these findings were revealed. Former patients are facing substantial suffering and expenses because they were never warned of the dangers related to Oxbryta.
December 3, 2024 - England Rejected Oxbryta From the Start
Before Pfizer decided to withdraw Oxbryta from the global drug market, it faced concerns from various health authorities around the world. Specifically, England's National Institute for Health and Care Excellence (NICE) advised Britain's National Health Service to reject Oxbryta approval based on a cost versus efficacy comparison.
Although Pfizer addressed some of NICE's concerns, the institute reported continued issues as recently as February 2024. By September, Pfizer pulled Oxbryta from the shelves. Unfortunately, many patients have already been harmed by this drug's side effects and face long-term medical problems and financial losses. The LLN team is pursuing these claims on behalf of injured patients and offers free consultations for anyone harmed by Oxbryta to discuss their legal options.
November 11, 2024 - Oxbryta Lawsuits Filed Against Pfizer and Global Blood Therapeutics Following FDA Recall
Two lawsuits have been filed against Pfizer and GBT over the serious risks of danger and death from Oxbryta.
In October 2024, Trebor Hardiman, a 67-year-old man, filed a complaint in a California state court alleging that Oxbryta caused him severe complications, including increased VOCs, debilitating pain, and a stroke.
His lawyers claim that GBT’s design, development, and marketing of Oxbryta were negligent because they failed to provide adequate warnings about the risks. The lawsuit seeks damages for strict liability, design defects, failure to warn, and breach of warranties.
Shortly after, on November 8, 2024, Tirrell Allen, an Illinois resident, filed a lawsuit in federal court, which now included Pfizer. Allen began to suffer severe VOCs and had a stroke, leading to his hospitalization. Allen only began taking Oxbryta in August 2024, just 3 months before he filed the lawsuit.
Both lawsuits accuse GBT and Pfizer of alleging that the companies knew or should have known about the serious risks associated with the drug but failed to communicate this to the public.
According to a memo about the cases, these lawsuits reflect a broader concern over GBT and Pfizer’s failure to adhere to safety protocols, accelerated FDA approvals, and their responsibility to patients. The Oxbryta lawsuits highlight a pattern of alleged negligence and misleading advertising. The outcome of these lawsuits could lead to further claims against Pfizer and GBT and may impact future regulatory actions on expedited drug approvals.

September 25, 2024: Pfizer Recalls Oxbryta Over Dangerous Side Effects
Pfizer announced a voluntary global recall of Oxbryta, a drug intended to treat sickle cell disease, following a series of new clinical data. These studies showed an increased risk of serious side effects, including a higher incidence of vaso-occlusive crises (VOCs), a painful event caused by red blood cells blocking blood flow, and, in some cases, death. These findings led Pfizer to conclude that Oxbryta’s risks now outweigh its potential benefits.
In response, Pfizer has stopped distributing Oxbryta and is advising people still taking it to consult with their doctor. This recall is a huge shift from Pfizer's earlier views on Oxbryta’s safety and effectiveness in managing sickle cell disease.

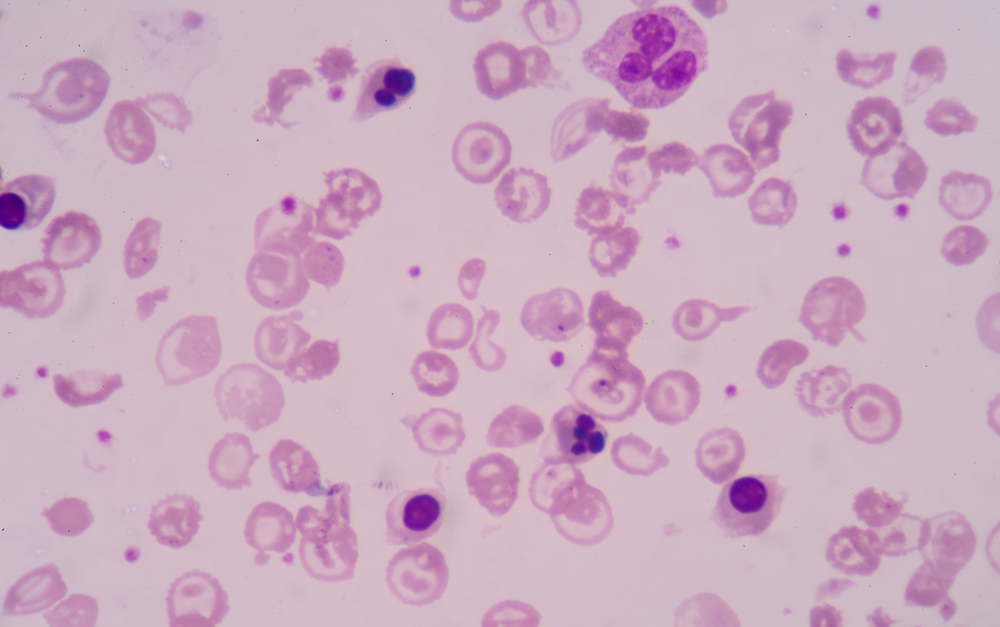
Oxbryta and Its Role in Sickle Cell Disease Treatment
Oxbryta (voxelotor) was first approved in 2019 as a promising new treatment for sickle cell disease (SCD), a hereditary condition affecting red blood cells' shape and function. Sickle cell disease causes red blood cells to become rigid and sickle-shaped, blocking blood flow and leading to serious complications, including severe pain, anemia, and organ damage. The introduction of Oxbryta provided hope for many patients, as it targeted the underlying cause of the disease rather than merely addressing the symptoms.
The drug works by increasing the ability of hemoglobin to carry oxygen, helping red blood cells maintain a regular shape, and reducing the likelihood of blockages in blood vessels. For patients struggling with the devastating effects of sickle cell disease, Oxbryta seemed like a breakthrough treatment. It was approved under the FDA’s accelerated approval pathway, which allows medications that address unmet medical needs to reach patients sooner, based on early clinical data.
Initially, Oxbryta was approved for patients aged 12 and older, but in 2021, its approval was expanded to include children as young as 4. This expansion was seen as a significant step forward, especially for families managing sickle cell disease in young children who had limited treatment options. However, as more data emerged through postmarketing studies and real-world use, the risks associated with Oxbryta began to overshadow its benefits.
Despite the initial optimism, postmarketing trials revealed that patients taking Oxbryta were experiencing higher rates of vaso-occlusive crises—a painful and dangerous complication of sickle cell disease—compared to those on a placebo.
These crises occur when sickled red blood cells block blood flow, depriving tissues of oxygen and causing severe pain. Along with the increased occurrence of VOCs, there were more deaths reported in the Oxbryta treatment group during these studies, raising serious concerns about the drug’s safety profile.
Based on these findings, Pfizer concluded that the risks of continuing Oxbryta use outweighed any potential benefits. The decision to voluntarily withdraw the drug was made to protect patients from further harm.
Ongoing Investigations and Legal Recourse
The withdrawal of Oxbryta followed a thorough review of postmarketing data, which uncovered significant safety concerns. Pfizer, the manufacturer of Oxbryta, conducted multiple postmarketing clinical trials and real-world studies to assess the long-term effects of the drug on patients with sickle cell disease. These studies revealed alarming trends that could not be ignored, prompting both the FDA and Pfizer to take action.
One of the most troubling findings was the increased rate of vaso-occlusive crises (VOCs) in patients taking Oxbryta compared to those taking a placebo. A VOC occurs when sickled red blood cells block blood vessels, cutting off oxygen to vital tissues and causing extreme pain. For patients who had hoped Oxbryta would alleviate their symptoms, this data was particularly distressing. Instead of providing relief, the drug appeared to exacerbate one of the most severe complications of sickle cell disease.

In addition to the increased risk of VOCs, the studies also revealed a higher mortality rate in patients treated with Oxbryta. This finding raised serious concerns about the overall safety of the medication. The increased risk of death, coupled with the worsened symptoms, led Pfizer to re-evaluate the drug’s risk-benefit profile. After reviewing the data, the company determined that the risks of continuing to distribute Oxbryta far outweighed its potential benefits for patients.
In collaboration with Pfizer, the FDA conducted its safety review, which included data from real-world registry studies and reports from the FDA Adverse Event Reporting System (FAERS). FAERS collects reports of adverse events from patients, healthcare professionals, and drug manufacturers, providing valuable insights into the safety of medications after they reach the market. The FDA’s analysis confirmed the concerning trends in Pfizer’s studies, reinforcing the decision to pull Oxbryta from the market.
In September 2024, Pfizer officially announced the voluntary withdrawal of Oxbryta. The company halted distribution of the drug and discontinued all ongoing clinical trials. The FDA promptly issued a public alert, advising healthcare professionals to stop prescribing Oxbryta and urging patients to consult their doctors about alternative treatments.
This swift action reflects the seriousness of the risks associated with Oxbryta. Both the FDA and Pfizer have emphasized the importance of ensuring patient safety, and this withdrawal marks a necessary step in protecting those affected by sickle cell disease from further harm.
What Patients and Healthcare Providers Should Do
Patients and healthcare providers must take immediate action in light of the FDA’s alert and Pfizer’s voluntary withdrawal of Oxbryta. The FDA has advised that doctors stop prescribing Oxbryta and transition their patients to alternative treatments. For patients taking Oxbryta, understanding the following steps and exploring other options with their healthcare providers is essential to ensure their health and safety.
Immediate Steps for Patients
If you or a loved one has been prescribed Oxbryta, the first and most important step is to contact your healthcare provider as soon as possible. Stopping medication should always be done under medical supervision, especially for those managing a complex condition like sickle cell disease. Abruptly discontinuing Oxbryta without consulting your doctor could lead to complications, as your body may need to adjust to the change in treatment.
The FDA recommends that patients work closely with their healthcare providers to find alternative therapies that are safer and better suited for their needs. Several FDA-approved medications are available to treat sickle cell disease, and your doctor will help determine the best option based on your medical history and current health status.
Alternative Treatments for Sickle Cell Disease
While Oxbryta may no longer be available, other effective treatments for sickle cell disease can help manage symptoms and improve quality of life. Some of the most common alternatives include:
- Hydroxyurea: This medication has been used for many years to reduce the frequency of painful vaso-occlusive crises and the need for blood transfusions in sickle cell patients. Hydroxyurea increases fetal hemoglobin production, which helps prevent red blood cells from becoming sickle-shaped.
- L-glutamine: Approved by the FDA in 2017, L-glutamine is another option for reducing the frequency of vaso-occlusive crises. It is an amino acid that helps reduce oxidative stress in red blood cells, making them less likely to sickle and cause blockages.
- Blood transfusions: Blood transfusions are a key part of managing sickle cell disease for some patients. Transfusions help increase the number of normal red blood cells in the bloodstream, reducing the risk of blockages and complications. While transfusions are not without risks, they can be a life-saving option for patients experiencing severe anemia or other complications.
- Bone marrow transplants: In some cases, a bone marrow transplant (also known as a stem cell transplant) may be an option to cure sickle cell disease. However, this procedure is complex and carries significant risks, including the potential for severe complications. It is generally reserved for patients with the most severe forms of the disease who have a suitable donor.
By working closely with their healthcare providers, patients can explore these and other treatment options to ensure they receive the care that best meets their needs. It’s also vital for patients and caregivers to stay informed about any new treatments or therapies that may become available in the future.
Legal Rights for Patients Affected by Oxbryta
The voluntary withdrawal of Oxbryta has left many patients questioning whether they have legal recourse for the harm caused by the medication. Pfizer’s decision to pull Oxbryta from the market after postmarketing studies revealed severe risks—including increased rates of vaso-occlusive crises and higher mortality—raises important questions about the company’s responsibility to the affected patients. For those who have suffered serious complications, understanding their legal rights is critical.
Understanding Pharmaceutical Liability
Pharmaceutical companies have a duty to ensure that the drugs they produce are safe and effective for patients. When a medication is linked to severe side effects or health risks that outweigh its benefits, the manufacturer may be liable for any harm caused. In the case of Oxbryta, patients who experience serious adverse effects such as vaso-occlusive crises, hospitalization, or the loss of a loved one due to the drug may have grounds to pursue a lawsuit.
One of the primary legal claims in cases like this is negligence. This occurs when a pharmaceutical company fails to act responsibly in ensuring the safety of its product. For instance, if Pfizer had information about Oxbryta’s risks but failed to take timely action to address these concerns or warn patients and healthcare providers, they could be held legally responsible for the injuries that occurred.
Another common legal claim in drug-related cases is failure to warn. Drug manufacturers are required to provide clear, accurate, and complete information about the potential risks associated with their medications. If Pfizer did not adequately inform patients or doctors about the dangers of Oxbryta—such as the increased risk of vaso-occlusive crises or death—then those who were harmed may be able to file a failure-to-warn lawsuit.
Potential Lawsuits for Oxbryta Injuries
Patients who were harmed by Oxbryta may be entitled to seek compensation through individual lawsuits. Each patient’s case is unique, and the damages they may recover will depend on the specific circumstances of their situation. Potential compensation claims can include:
- Medical Expenses: Patients may be able to recover compensation for any medical costs incurred as a result of Oxbryta’s side effects. This includes hospitalizations, treatments for vaso-occlusive crises, and ongoing medical care related to the drug's complications.
- Pain and Suffering: Beyond the physical harm, patients may also seek compensation for the emotional and physical pain they endured due to Oxbryta. Severe pain from vaso-occlusive crises and the emotional toll of dealing with worsening symptoms can be significant factors in these claims.
- Lost Income or Earning Capacity: If Oxbryta’s side effects caused a patient to miss work or left them unable to continue their job, they may be entitled to compensation for lost wages or diminished earning potential.
- Wrongful Death Claims: In cases where Oxbryta led to the death of a loved one, families may pursue a wrongful death lawsuit. These claims can seek compensation for funeral expenses, loss of companionship, and the financial support the deceased would have provided.
Patients and families should act quickly if they believe they have a potential legal claim. Each state has specific statutes of limitations that limit the time a patient has to file a lawsuit after discovering that a drug caused them harm. Acting within these timeframes is essential to preserving the right to pursue compensation.
Class Action vs. Individual Lawsuits
Many patients may consider participating in a class action lawsuit when a drug like Oxbryta is withdrawn from the market due to safety concerns. While class actions can be practical for cases where many people have experienced similar harm, they may not be the best option for everyone, particularly for those who have suffered serious injuries.
In a class action lawsuit, one or more plaintiffs represent a larger group of people harmed similarly. These cases are often used when the individual claims are too small to justify separate lawsuits.
However, regarding pharmaceutical injuries, each patient’s case is unique. Factors such as the severity of the side effects, the medical treatments required, and the overall impact on a patient’s life can vary significantly. As a result, patients who have been seriously harmed by Oxbryta may be better served by filing an individual lawsuit.
Individual lawsuits allow patients to seek compensation based on their specific circumstances. Unlike a class action, where the payout is typically distributed equally among all participants, an individual lawsuit can account for the unique damages each patient has suffered. This could lead to a higher payout for those who experienced more severe injuries or long-term complications.
How Legal Representation Can Help
Navigating pharmaceutical liability cases is complex, especially when dealing with postmarketing drug withdrawals like Oxbryta. These cases often require a detailed investigation, expert testimony, and a comprehensive understanding of both medical and legal issues. For patients and families dealing with the devastating effects of Oxbryta, seeking experienced legal representation is crucial.
An attorney with expertise in pharmaceutical liability can help evaluate whether a patient has a valid claim, gather the necessary evidence to build a strong case and pursue the maximum compensation available. These cases often involve reviewing medical records, clinical trial data, and FDA reports to establish that the manufacturer was responsible for the harm caused.
Moreover, taking on large pharmaceutical companies like Pfizer requires resources and legal experience. Patients may find obtaining the compensation they deserve easier with skilled legal representation. By working with an experienced lawyer, patients can ensure that their rights are protected and they have a fair chance at receiving justice.
The Importance of Ongoing Medical Monitoring
Even after stopping Oxbryta, patients should monitor their health closely and attend regular medical checkups. Sickle cell disease is a lifelong condition that requires ongoing management to prevent complications and maintain quality of life. Patients should also report any new or worsening symptoms to their healthcare providers, as this could indicate the need to adjust their treatment plan.
Healthcare providers play a critical role in guiding patients through this transition. In addition to prescribing alternative treatments, doctors should monitor patients for any lingering effects of Oxbryta and provide support as they adapt to new therapies. This collaborative approach between patients and healthcare providers is essential for managing sickle cell disease effectively and safely.
To Learn More About an Oxbryta Lawsuit, Contact Lawsuit Legal News
If you or a loved one was harmed by taking Oxbryta, it’s important to speak with a qualified Oxbryta product recall lawyer who understands the complexities of pharmaceutical lawsuits. Our team at Lawsuit Legal News is ready to assist you in building a strong case against those responsible.
Working with an experienced legal team can make all the difference in gathering the evidence you need to file a successful Oxbryta lawsuit. Contact our attorneys today to explore your legal options and determine if you can seek compensation for the harm you’ve suffered.
We are prepared to help you navigate the legal process and pursue justice for the injuries caused by Oxbryta. Contact Lawsuit Legal News at (833) 552-7274 or online to learn if you qualify to file an Oxbryta lawsuit and hold Pfizer accountable.